Neuroforaminal stenosis, also known as stenosis of the neuroforamen or simply foraminal stenosis, is a common condition in which one or more of the openings through which the spinal nerve roots pass decreases in size at a given vertebral level. Stenosis may occur unilaterally or bilaterally at any given spinal location and may eventually cause what is commonly known as a pinched nerve. It must be noted immediately that stenosis of the neuroforaminal spaces is not inherently problematic or symptomatic. In fact, this condition is a normal, typical and expected part of spinal aging, particularly in the cervical and lumbar areas of the spine.
This resource section will provide a comprehensive overview of stenotic neuroforamen and will also explain the condition in depth in the additional article topics contained herein.
Neuroforaminal Stenosis Defined
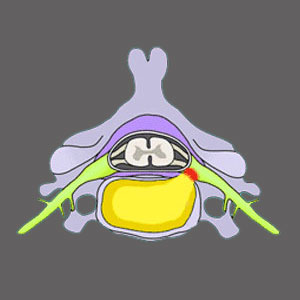
Neuroforamen exist at every normal vertebral level. They are spaces on the sides of each bone which allow nerve roots to pass as they exit the spinal canal. These nerve roots go on to form a complex and extensive network of neurological tissues which serve the sensory and motor needs of almost the entire body.
Imagine the foramen as being windows on both sides of the spinal canal. Nerves must exit through these windows, but sometimes, one or many of these windows can shut slightly or completely. This is foraminal stenosis. Stenosis of the foraminal spaces is a condition diagnosed when the opening is narrowed, partially closed off or virtually sealed shut.
In minor to moderate cases of stenosis, there is not likely to be any symptoms, since the nerve still has plenty of room to exit freely without compression. In very severe cases, where the foraminal space is almost totally closed off, the nerve may become compressed, leading to foraminal stenosis symptoms in the area of the body served by that particular neurological structure.
Learn all about cervical foraminal stenosis and lumbar foraminal stenosis, the 2 most common locations for canal narrowing to occur. Only in rare instances does thoracic foraminal stenosis reach symptomatic levels.
Foraminal Stenosis Conditions
There are many causes of foraminal stenosis which may enact narrowing and are commonly diagnosed using MRI or CT testing. Just like in central spinal stenosis conditions, there are causes which are related to bone changes, called permanent changes and alterations of the foraminal space related to soft tissue pathologies, such as herniated discs, which are transitory stenosis conditions.
There are no inherent symptoms of foraminal stenosis, since the condition itself is not painful unless it compresses a nerve root. Even when a pinched nerve does occur, the result is rarely chronic pain, as is often mistakenly perceived. Instead, the end result is true and objective weakness and numbness in the affected tissues served by that compressed nerve. Learn why a person might demonstrate narrow neuroforamen.
Nerve root impingement can occur in several degrees that may or may not become symptomatic. Foraminal stenosis is the most common causation of nerve impingement, but other types of stenosis can cause nerve root compression, as well.
Neuroforaminal Stenosis Guidance
Just like with central spinal stenosis, there are not many effectual nonsurgical treatments for foraminal stenosis, particularly if the root cause is related to advanced arthritic change in the affected area. However, surgery should only be considered if the diagnosis is absolutely verified and the patient has no other options left.
It is crucial to mention that of all spinal conditions, pinched nerves are some of the most often misdiagnosed, helping to explain the horrific curative results offered by most conservative and surgical therapy options. In the vast majority of cases where are pinched nerve is mistakenly identified due to foraminal stenosis, the symptoms do not correlate and the structural findings do not adequately support the diagnostic theory. This means that in the majority of patients, sure there is some narrowing of the foraminal opening, but not enough to justify any symptoms.
Additionally, the pain which exists does not correlate to the mistakenly implicated nerve in many patients. In fact, almost all misdiagnosed cases of stenosis of the neuroforamen involve symptomatic expressions which are too diverse to possibly come from the culprit condition.
If you are confident that your diagnosis is accurate, then it is time to consult with your neurologist to explore the best foraminal stenosis treatment for your particular case profile. Before making a final therapy selection, be sure to fully understand the risks and rewards of foraminal stenosis surgery.
Foraminal Stenosis Factsheet
Sure you may have the structural changes associated with foraminal narrowing clearly visible on an MRI report. However, unless the space is almost complete closed off, then the mild to moderate stenosis is probably not responsible for doing any damage whatsoever. Of course, when the stenosis is severe, there may surely be a true pinched nerve condition which may require aggressive or even drastic surgical intervention in order to restore functionality to the affected region.
In order to better your odds of successful symptomatic resolution, always consult with a spinal neurologist for diagnosis and treatment when foraminal stenosis is the working diagnostic theory. Read more about foraminal narrowing being blamed for causing back or neck pain.
Our Cure Back Pain Forever Program is very effective for reducing pain due to neuroforaminal stenosis. You can get help immediately, since our program is available around the clock from anywhere in the world.
Spinal Stenosis > Neuroforaminal Stenosis