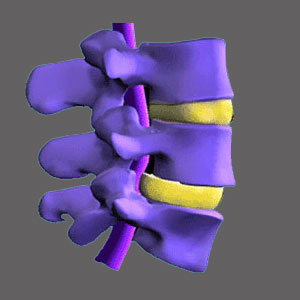
Lateral spinal stenosis goes by many other names, including lateral recess stenosis and subarticular stenosis. This condition is very similar to foraminal stenosis in that it does not affect the patency of the central spinal canal, but instead potentially affects the functionality a single nerve root exiting the spinal canal. While foraminal stenosis describes a condition in which the nerve root is possibly compressed as it leaves the neuroforaminal space, lateral stenosis may involve compression of the nerve root before it approaches the neuroforamen. This form of stenotic change is most common in the lumbar spine, but can also occur in the cervical spine, as well.
This article will examine the potential for pinched nerves to occur due to lateral recess stenosis and the types of structural causes which generally enact symptoms.
Lateral Spinal Stenosis or Foraminal Stenosis
In scenarios involving neuroforaminal stenosis, the opening of the nerve foramen is narrowed. Meanwhile, in the lateral stenosis diagnosis, the passageway from the central canal to the neuroforaminal opening is narrowed. The causes of both conditions can be exactly the same, as can the potential symptoms.
Remember that just because the lateral recess is narrowed does not mean that symptoms will occur. In fact, this type of stenosis is the variety which rarely causes pain or related neurological symptoms to occur. This is because the space though which the nerve passes on the way out of the spinal canal is much larger than it needs to be, so even moderate stenosis of the lateral recess will not produce any symptoms in most patients.
Lateral Stenosis or Far Lateral Stenosis
Far lateral stenosis occurs after the nerve root has passed through the foraminal space, completely exiting the spinal canal. This event is probably the least often seen or diagnosed, but is certainly possible, particularly in association with far lateral herniated discs.
In these cases, the nerve root affected will be the one above the herniated disc, instead of the one at the same level, as expected.
Far lateral stenosis may not show up on many MRI scans leading to a misdiagnosed condition and very poor treatment results. Symptomatic correlation and nerve conduction testing are some of the best ways of diagnosing suspected far lateral stenosis concerns.
Lateral Spinal Stenosis Guidance
I understand that the terminologies used can be very confusing for many patients and some doctors do not do an adequate job of explaining the diagnosis. It is important that all patients do indeed understand their theorized cause of pain, so that they can take an active role in their treatment and comprehend exactly what is happening during every step of the process.
In lateral recess stenosis cases, time may alleviate the condition or more proactive measures may need to be taken when a nerve is actually pinched. Just be sure to understand that narrowing of the lateral recess is an extremely common event in the lower lumbar spine and is also often seen in the middle to lower cervical spine, as well.
Just because the recess is decreased in size does not mean that the causative source has been definitively located. Only neurological correlation, nerve conduction analysis or an actual image or visualization of the compressed nerve will really help pinpoint the diagnosis as correct. Barring these, the pronouncement of lateral stenosis is often nothing more than a guess, based on virtually universal anatomical changes.
Spinal Stenosis > What is Spinal Stenosis? > Lateral Spinal Stenosis